Rheumatoid arthritis affects 1 in 100 people worldwide. It causes inflamed, painful, and swollen joints, often in the hands and wrists, and can lead to loss of joint function, chronic pain, and joint deformity and damage. What causes this condition is unknown.
In our recently published study, my colleagues and I found an important clue to a possible culprit behind this disease: the bacteria in your gut.
What causes rheumatoid arthritis?
Rheumatoid arthritis is an autoimmune disease, meaning it develops when the body’s immune system starts attacking itself. Proteins called antibodies that normally help fight off viruses and bacteria begin attacking the joints instead.
The origins of the antibodies that cause rheumatoid arthritis have been an area of research for many years. Some research has shown that these antibodies can build up in places like the mouth, lungs, and intestines for more than 10 years before symptoms appear. However, until now it was unclear why researchers found these antibodies in these specific areas.
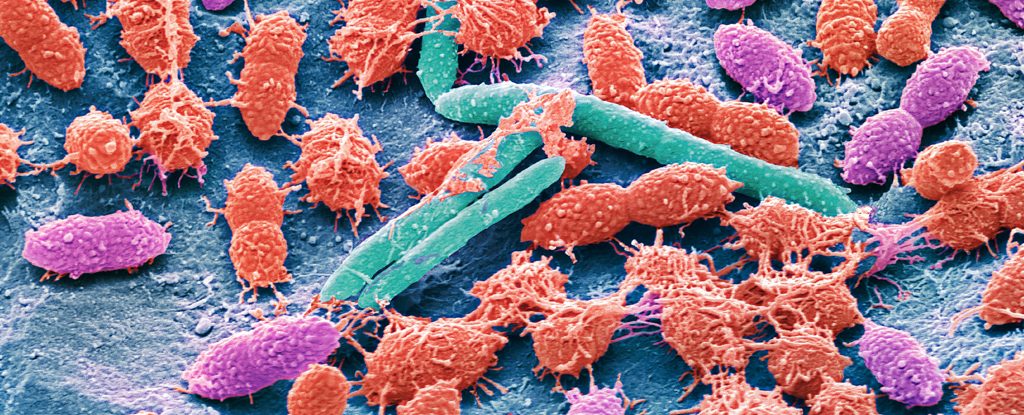
We wanted to investigate what could trigger the formation of these antibodies. Specifically, we wondered if bacteria in the microbiome, a community of microorganisms that live in the gut, might be the ones activating the immune response that leads to rheumatoid arthritis.
Because microbes generally live in the same places as the antibodies that drive rheumatoid arthritis, we hypothesized that these bacteria might trigger the production of these antibodies. We reasoned that although these antibodies should attack the bacteria, when they spread beyond the gut and attack the joints, rheumatoid arthritis develops.
First, we tried to identify the gut bacteria targeted by these antibodies. To do this, we exposed the bacteria in the faeces of a subset of people at risk of developing rheumatoid arthritis to these antibodies, allowing us to isolate only the bacterial species that responded to and bound to the antibodies.
We found that a previously unknown type of bacteria was present in the gut of about 20 percent of people who were either diagnosed with rheumatoid arthritis or who produce antibodies that cause the disease.
As a member of the Cherokee Nation of Oklahoma, I suggested naming this species Subdoligranulum didolesgii (“didolesgii” means arthritis or rheumatism in Cherokee) as a nod to the contributions other Indigenous scholars have made to science, as well as the fact that rheumatoid arthritis affects Indigenous peoples more frequently than other populations.
Subdoligranulum didolesgii has not been detected in the faeces of healthy people and it is currently unknown how common this bacterium is in the general population.
We also found that these bacteria can activate specialized immune cells called T cells in people with rheumatoid arthritis. T cells drive inflammatory responses in the body and have been implicated in the development of various autoimmune diseases.
These results suggest that these gut bacteria could activate the immune system of people with rheumatoid arthritis. But instead of attacking the bacteria, their immune system attacks the joints.
frameborder=”0″ allow=”accelerometer; autoplay; write clipboard; encrypted media; gyroscope; picture-in-picture” allow full screen>
Why these bacteria?
It is still unknown why people with rheumatoid arthritis develop an immune response to it Subdoligranulum didolesgii. But we think it could be the culprit when it comes to rheumatoid arthritis because this bacterium is only found in the gut of people with rheumatoid arthritis and not in the gut of healthy people.
While many immune responses occur in the gut, they are usually self-contained and do not spread to other areas of the body. However, we believe that a particularly strong intestinal immune response speaks against it Subdoligranulum didolesgii could allow antibodies to bypass the intestinal “firewall” and spread to the joints.
To confirm our hypothesis, we gave mice an oral dose of Subdoligranulum didolesgii and watched her reaction. Within 14 days, the mice began developing joint swelling and antibodies attacking their joints.
The future of rheumatoid arthritis treatment
My colleagues and I hope this research can shed light on the origins of rheumatoid arthritis. Our next goal is to find out how common these bacteria are in the general population and to test whether the presence of these bacteria in the gut can lead to the development of rheumatoid arthritis in humans.
It’s important to note that antibiotics are unlikely to be a helpful treatment for the microbiomes of rheumatoid arthritis patients. Even though Subdoligranulum didolesgii While some people with rheumatoid arthritis can trigger an autoimmune response, antibiotics eliminate both helpful and harmful bacteria in the gut. Additionally, removing the bacteria will not necessarily stop the immune system from attacking the joints once it has started.
Nonetheless, we believe these bacteria can be used as tools to develop treatments for rheumatoid arthritis and hopefully ways to prevent the disease.
Meagan Chriswell, MD/PhD student in Immunology, University of Colorado Anschutz Medical Campus
This article was republished by The Conversation under a Creative Commons license. Read the original article.
#Newly #discovered #gut #microbe #trigger #rheumatoid #arthritis

Leave a Comment