“I just can’t do what I used to do anymore.”
As pulmonologists and critical care physicians treating patients with lung disease, we have heard many of our patients who have recovered from COVID-19 say so months after their initial diagnosis. Although they have survived what may be the most life-threatening phase of their illness, they have yet to return to their pre-COVID-19 status, struggling with activities ranging from strenuous exercise to doing laundry.
These ongoing effects, dubbed Long COVID, have affected up to one in five American adults diagnosed with COVID-19.
Long COVID includes a variety of symptoms such as brain fog, fatigue, cough and shortness of breath.
These symptoms can result from damage or dysfunction of multiple organ systems, and understanding the causes of a long COVID is a particular research focus of the Biden-Harris administration.
Not all breathing problems are related to the lungs, but in many cases the lungs are affected.
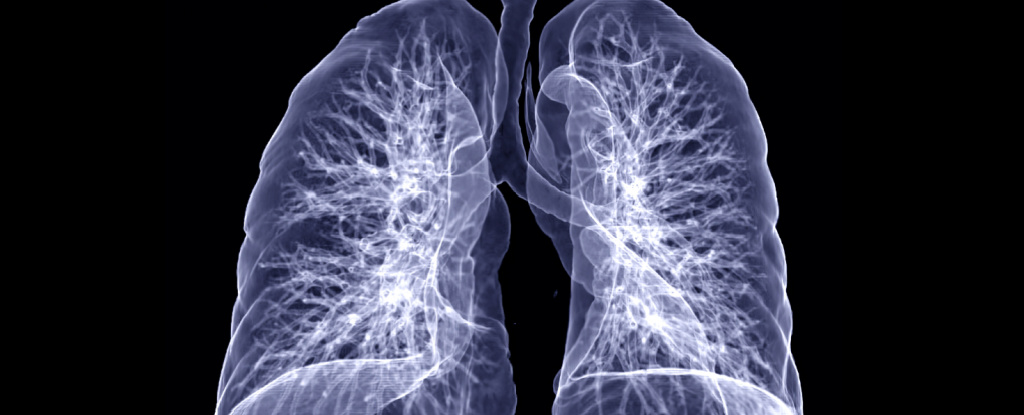
Looking at the basic functions of the lungs and how disease can affect them can help clarify what’s on the horizon for some patients after COVID-19 infection.
Normal lung function
The main function of the lungs is to bring oxygen-rich air into the body and expel carbon dioxide. When air enters the lungs, it is brought into close proximity with the blood, where oxygen diffuses into the body and carbon dioxide diffuses out.
frameborder=”0″ allow=”accelerometer; autoplay; write clipboard; encrypted media; gyroscope; picture-in-picture” allow full screen>
This process, simple as it sounds, requires extraordinary coordination of airflow or ventilation and blood flow or perfusion.
There are over 20 divisions in your airways, starting with the main windpipe, or trachea, and ending with the small balloons at the end of the airways called alveoli, which are in close contact with your blood vessels.
When an oxygen molecule reaches the end of the airway, there are about 300 million of these small alveoli where it could end up, with a total area of over 1,000 square feet (100 square meters) where gas exchange takes place.
Matching ventilation and perfusion rates is critical to basic lung function, and damage along the airways can lead to breathing difficulties in a number of ways.
Obstruction – reduced airflow
One form of lung disease is obstruction of airflow in and out of the body.
Two common causes of such impairments are chronic obstructive pulmonary disease and asthma.
In these conditions, the airways narrow either from damage from smoking, as is common in COPD, or from allergic inflammation, as is common in asthma. In both cases, patients have difficulty purging air from their lungs.
Researchers have observed persistent airflow obstruction in some patients who have recovered from COVID-19.
This condition is typically treated with inhalers that deliver drugs that open the airways. Such treatments can also be helpful during recovery from COVID-19.
Restriction – reduced lung volume
Another form of lung disease is called restriction or difficulty expanding the lungs. The restriction reduces the volume of the lungs and consequently the amount of air they can hold.
A limitation often results from the formation of scar tissue, also called fibrosis, in the lungs due to injury.
Fibrosis thickens the walls of the air sacs in the lungs, making it difficult for gas to exchange with the blood.
This type of scarring can occur in chronic lung diseases such as idiopathic pulmonary fibrosis or as a result of severe lung damage in a condition called acute respiratory distress syndrome or ARDS.
ARDS can be caused by injuries that originate in the lungs, such as B. pneumonia, or severe diseases in other organs, such. B. Pancreatitis. About 25 percent of patients who recover from ARDS develop restrictive lung disease.
Researchers have also found that patients who have recovered from COVID-19, particularly those who have had serious illness, may later develop restrictive lung disease.
COVID-19 patients who require ventilators may also have similar recovery rates to those who require ventilators for other conditions. The long-term recovery of lung function in these patients is still unknown. Drugs to treat post-COVID-19 fibrotic lung disease are currently undergoing clinical testing.
Impaired Circulation – Decreased blood flow
Finally, even if airflow and lung volume are unaffected, the lungs cannot perform their function if blood flow to the alveoli, where gas exchange occurs, is impaired.
COVID-19 is associated with an increased risk of blood clots. If blood clots travel to the lungs, they can cause a life-threatening pulmonary embolism, which restricts blood flow to the lungs.
Over the long term, blood clots can also cause chronic poor circulation in the lungs, a condition called chronic thromboembolic pulmonary hypertension, or CTEPH.
Only 0.5 to 3 percent of patients who develop a pulmonary embolism for reasons other than COVID-19 develop this chronic problem.
However, there is evidence that severe COVID-19 infections can directly damage the blood vessels in the lungs and affect blood flow during recovery.
What’s next?
Lungs can function less than optimally in these three general ways, and COVID-19 can lead to all of them. Researchers and clinicians are still looking for ways to best treat the long-term lung damage seen in long COVID.
For clinicians, close follow-up of patients who have recovered from COVID-19, particularly those with ongoing symptoms, can result in a faster diagnosis of long-term COVID-19.
Severe cases of COVID-19 are associated with higher rates of long-staying COVID. Other risk factors for developing a long COVID include pre-existing type 2 diabetes, the presence of viral particles in the blood after initial infection, and certain types of abnormal immune function.
For researchers, Long COVID is an opportunity to study the underlying mechanisms of how different types of lung diseases resulting from COVID-19 infection develop.
Uncovering these mechanisms would allow researchers to design targeted treatments to speed recovery and get more patients feeling and breathing like they did before the pandemic.
In the meantime, everyone can keep up to date on recommended vaccinations and use preventive measures such as good hand hygiene and masks if necessary.![]()
Jeffrey M. Sturek, Assistant Professor of Medicine, University of Virginia and Alexandra Kadl, Assistant Professor of Medicine and Pharmacology, University of Virginia.
This article was republished by The Conversation under a Creative Commons license. Read the original article.
#short #breath #ways #COVID19 #longterm #damage #lungs

Leave a Comment