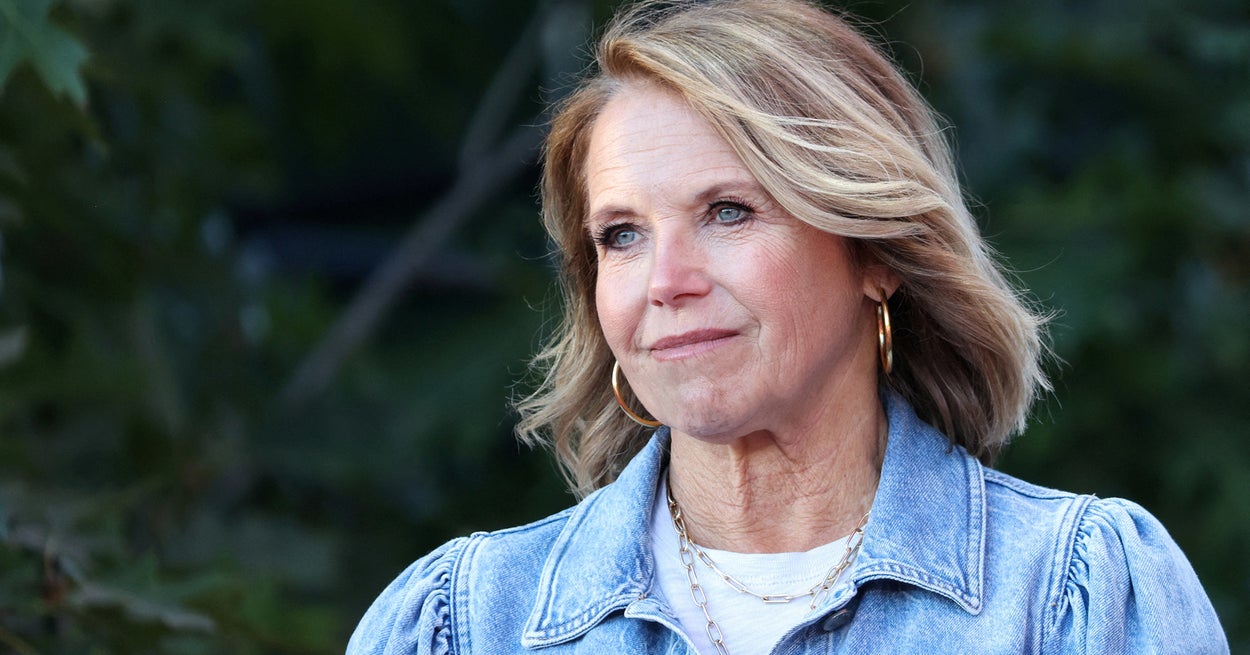
Katie Couric, a longtime colonoscopy proponent, is now advocating breast cancer screening after a routine mammogram and ultrasound in June revealed she had a tumor herself.
After a successful lumpectomy and radiation treatment, the 65-year-old journalist uses her experience to emphasize the importance of breast cancer awareness as we celebrate Breast Cancer Awareness Month this October. Breast cancer, affecting 1 in 8 women, is the most common non-skin cancer in women and the second-deadliest cancer for women, right after lung cancer.
Couric said she was six months overdue for her mammogram and intended to film it to raise awareness of the screening procedure, as she did at the time today Show filmed her colonoscopy in 2000. (Her first husband, Jay Monahan, died of colon cancer in 1998.)
“If I forgot to make an appointment for a mammogram, this might be a helpful reminder for others as well,” she wrote in an essay on her website. The reminder is especially needed now that mammography rates have fallen during the pandemic.
However, her diagnosis of a stage 1A olive-sized tumor shed even more light on the problem. “Please do your annual mammogram. I was six months late this time. I shudder to think of what would have happened if I had delayed it longer,” she wrote. “But just as importantly, please find out if you need additional screening.”
Couric also had an ultrasound, which is recommended for people with dense breasts. Breast density, which is unrelated to the size of your breasts, is an additional risk factor for breast cancer because it can make it more difficult to detect cancer on a mammogram. Luckily her cancer hadn’t spread anywhere else and she didn’t need chemotherapy.
Bethany Kandel, a New York City-based author and founder of breast cancer resource website BreastCancerFreebies.com, had a similar experience.
“Like Katie, I put off my yearly mammogram/sonogram — I have dense breasts,” she said. She was only two months overdue, in good health and just turned 50. “And when I finally left, there was a small cancerous tumor. I ended up having to have surgery – a lumpectomy like Katie – chemotherapy and radiation.” However, Kandel wonders if she would have needed the chemo had she left sooner.
“I wrestled with it for a while,” she said. “I was scared before it turned out to be nothing, so I wasn’t worried. I should have left earlier. The result might have been the same, but I wouldn’t have felt the guilt that I ended up carrying.” Kandel has been cancer-free for 15 years.
There is no question that mammograms have become an important part of healthcare. “Breast cancer screening saves lives,” said Dr. Ruth Oratz, a breast cancer oncologist at NYU Langone’s Perlmutter Cancer Center. “Because Katie Couric went for a screening mammogram, her breast cancer was discovered when it was young and curable.”
The death rate from breast cancer fell by 40% between 1990 and 2017 as awareness campaigns drew attention to mammograms. “Recent advances in the treatment and improvement in survival for breast cancer are due in part to routine screening,” said Dr. Nancy Chan, medical oncologist and director of clinical breast cancer research, also at NYU Langone’s Perlmutter Cancer Center.
When should you start having routine mammography screenings?
When to start mammography and how often to get it can vary a bit depending on which medical organization is making the recommendation.
For example, the US Preventive Services Task Force says the decision to start mammograms under age 50 is an “individual decision” and people over 50 should have them every two years; the American Cancer Society offers a choice under age 45, but then recommends annual mammograms from age 45; The American College of Physicians says the potential harms of mammograms outweigh the benefits for most people between the ages of 40 and 49, and recommends screening every six months for those over 50.
Mammograms require a small amount of radiation, and because the risk of breast cancer increases with age, starting regular screening early can, in some cases, result in unnecessary testing or biopsies – and the associated psychological distress.
“Different medical organizations have different approaches,” said Jessica Leung, MD, professor of breast imaging at the University of Texas MD Anderson Cancer Center. You can use different data or analysis methods. “But perhaps most importantly, they may have different concepts of benefit versus risk or harm,” she said. “For example, patient anxiety is considered a risk for mammography screening. But how do you quantify that risk versus the benefit of saved lives?”
Many doctors recommend annual mammograms for people aged 40 and older who have an average breast cancer risk. As a general rule, you should start talking to your doctor when you turn 40, although you may have this conversation sooner if you have certain risk factors. (For example, if you had a family history of breast cancer, inherited a BRCA1 or BRCA2 gene mutation, or had radiation therapy to the breast between the ages of 10 and 30, you might start earlier.)
“In general, we recommend a baseline mammogram around age 40 and once a year thereafter,” Oratz said. dr Sheldon M. Feldman, director of the breast surgery and breast surgical oncology program and director of breast cancer services at Montefiore Einstein Cancer Center, also says it should start at age 40 unless there is a history of breast cancer in close family members.
“Mammograms allow for earlier diagnosis and improved survival with less aggressive treatment,” he said, which may mean that if you get it early enough, you can avoid chemo or a mastectomy.
like dr Leung is following American College of Radiology guidelines for Christine Staeger-Hirsch, attending physician for breast imaging at Montefiore Health System.
“There are other policies out there [but] We believe the best and most comprehensive protocol is annual mammography screening, starting at age 40 and continuing beyond 75 as long as you are otherwise in good health,” she said. “It’s so important to get your yearly mammogram so that small, subtle changes can be spotted earlier.” Although survival rates are similar at an early or later stage, she said, “individual treatment is easier for the patient at an earlier stage .”
If you have dense breasts, you may need additional testing
#Katie #Courics #cancer #diagnosis #sheds #light #breast #density #important #mammograms

Leave a Comment