The retrospective data raise hope that ongoing randomized trials will demonstrate benefit in this subset of acute stroke patients.
Retrospective data from a German registry suggest that patients with acute ischemic stroke who are hospitalized with a delay and who already have large cerebral infarctions may also benefit from endovascular therapy to remove the clot.
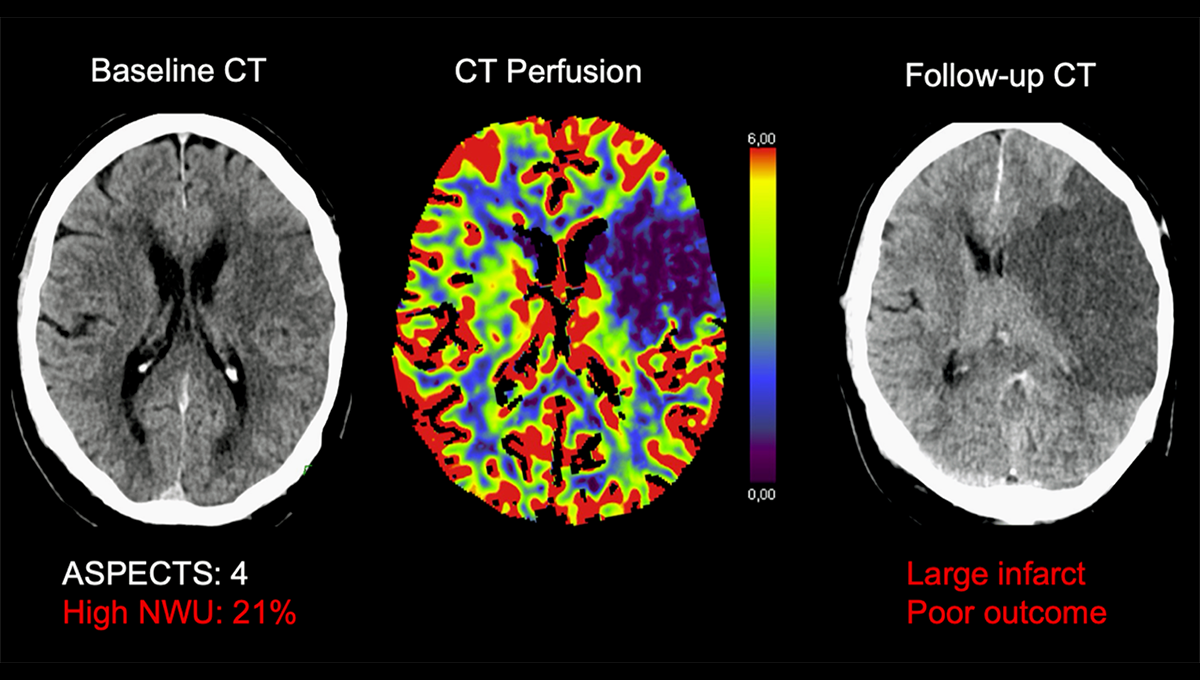
Among patients treated more than 6 hours after stroke onset and who had extensive evidence of infarction on CT (ASPECTS 5 or less), those who had good recanalization after stroke thrombectomy were more likely to have favorable functional outcome – defined as a modified Rankin scale (mRS) score of 0-3 – at 90 days were those whose vessel was not adequately opened (32% vs. 13%).
Other outcomes, including functional independence (mRS score 0-2) at 90 days and early neurological improvement, also appeared to be supported by the procedure, according to researchers led by Gabriel Broocks, MD (University Hospital Hamburg-Eppendorf, Hamburg, Germany ). , report in an article recently published online in JAMA network open.
The study highlights a new segment of acute ischemic stroke patients who could benefit from endovascular therapy if results are confirmed in ongoing studies. Although previous studies have both demonstrated the safety and effectiveness of mechanical thrombectomy within 6 hours of onset of symptoms and up to 24 hours after the onset of the strokewith selection based on imaging, they mostly excluded patients with large cerebral infarctions at baseline.
RESCUE-Japan LIMITreported earlier this year showed that endovascular therapy improved functional outcomes in patients with large ischemic nuclei (ASPECTS 3-5), although most patients were admitted within 6 hours of stroke onset.
Therefore, uncertainty remains about patients who present both late and have large infarcts, a group included in several studies that are in the process of enrollment or have recently completed enrollment, including VOLTAGE, TESLA, CHOOSE2and ANGEL ASPECT.
In that regard, Broocks told TCTMD, these retrospective data, limited by potential selection bias and the lack of a control group of patients who did not undergo thrombectomy, are “very encouraging for the studies that are currently ongoing.”
Indeed, commented Ashutosh Jadhav, MD, PhD (Barrow Neurological Institute, Phoenix, AZ), the release of this paper was well timed. Although the study has the usual limitations of a registry analysis, he said: “I think it shows promise and certainly gives confidence that the ongoing studies or completed studies will show benefit. And so it’s kind of a bridge until we get to the results of the randomized controlled trial data.”
German Stroke Registry – Endovascular Treatment
For the study, Broocks et al. to the German Stroke Registry – Endovascular Treatment, which contains information collected from 25 stroke centers across Germany. The current analysis focused on 285 patients (mean age 73 years; 51% males) who underwent mechanical thrombectomy between July 2015 and December 2019, had a large cerebral infarction (ASPECTS of 5 or less) and 6 to 24 hours post-stroke occurred beginning.
Successful recanalization, defined as a modified TICI score of 2b or 3, was achieved in 75% of patients. This was associated with significantly higher probabilities of the following outcomes:
- Favorable functional outcome at 90 days (adjusted OR 4.39; 95% CI 1.79-10.72)
- Functional independence at 90 days (adjusted OR 7.24; 95% CI 2.01-26.09)
- Early neurological improvement (adjusted OR 2.49; 95% CI 1.15-5.37)
Inverse probability weighting analyzes showed that successful recanalization was associated with relative increases in the odds of a favorable outcome (by 19%), functional independence (by 16%), and early neurological improvement (by 14%).
Further analysis suggested that recanalization improves outcomes in time windows up to 17.6 hours after stroke onset and in patients with ASPECTS 3-5.
The overall rate of secondary symptomatic intracerebral hemorrhage was relatively low at 6.3%, suggesting that “endovascular treatment may be safe for these specific patients,” Broocks said.
Defining the limits of endovascular therapy
It is known that vessel opening is generally good in patients with large vessel occlusions, and now researchers are aiming to define situations for which there may or may not be a benefit from endovascular therapy, Jadhav said.
Patient groups of particular interest are those with an NIHSS score < 6, those with more distal occlusions, and those with large ischemic nuclei. The field comes closest to answering whether intervention is beneficial in this latter patient population and whether the overall ASPECTS cutoff for eligibility should be around 3, Jadhav said, noting that ANGEL-ASPECT in China and TESLA in North America recently have completed the registration.
Some of these patients with large infarctions are already being treated off-label, with large differences between centers and regions, he observed. “That’s why we’re doing the trials to harmonize practice patterns and have better quality data to justify one approach or another.”
There is certainly confidence that the ongoing studies or completed studies will show a benefit. Ashutosh Jadhav
Some physicians might justify intervention in these patients based on evidence of benefit in certain studies and knowledge of poor outcomes and complications associated with no treatment, Jadhav added. “I think if people are currently doing this off-label, it’s because we know the alternative in these patients. If you don’t open the blood vessel, it can be pretty devastating.”
If the ongoing studies demonstrate the safety and efficacy of thrombectomy in patients presenting late and/or with large infarcts, “the impact will be quite significant because we are will see an increase in the number of procedures performed,” Jadhav said.
He pointed a summary He and colleagues presented an estimate at the International Stroke Conference 2022 in February that 18,484 adults met stringent eligibility criteria for endovascular therapy in 2021 and that an additional 9,621 with poor imaging (large ischemic core) could be eligible each year. if ongoing studies show a benefit. And in another study from his group, published in Stroke In 2018, approximately 25% of patients who did not meet criteria for late window thrombectomy were excluded due to poor imaging.
Going forward, Broocks said, it will be important to further refine patient selection within the large infarct subgroup to identify those who benefit most and also to determine if there is a difference in patient selection across the subgroup basis of CT or MRI there.
#Stroke #thrombectomy #work #large #infarcts #late #window

Leave a Comment