Since the first cases of monkeypox were reported in Canada in May, the number of reported cases across the country has risen to 890 as of Wednesday.
The World Health Organization has declared monkeypox a public health emergency of international concern, meaning the disease has the potential for further international spread that may require a coordinated global response. And the U.S. government on Thursday declared it a public health emergency and signaled it will deploy more resources to deal with the surge in cases.
To understand the risks of an illness that causes symptoms like fever, headache, swollen lymph nodes and a painful rash or skin lesions, The Globe sought expert advice on how to manage this outbreak.
How is monkeypox transmitted?
In the current global outbreak, almost all cases of monkeypox have been spread through close, intimate person-to-person contact, predominantly among men who have sex with men.
According to the WHO, this can happen through respiratory droplets, contact with skin lesions from an infected person, or contact with recently contaminated items such as bedding and clothing. According to the WHO, transmission via respiratory droplets usually requires prolonged personal contact.
It is still unclear whether the virus can be transmitted through sexual fluids. A new study in The Lancet Infectious Diseases suggested this might be the case, finding prolonged release of monkeypox DNA in semen, suggesting a viable virus, although more research is needed.
Analysis: As cases of monkeypox rise worldwide, experts say it’s unclear whether the outbreak can be contained
How long does the virus live outside the human body?
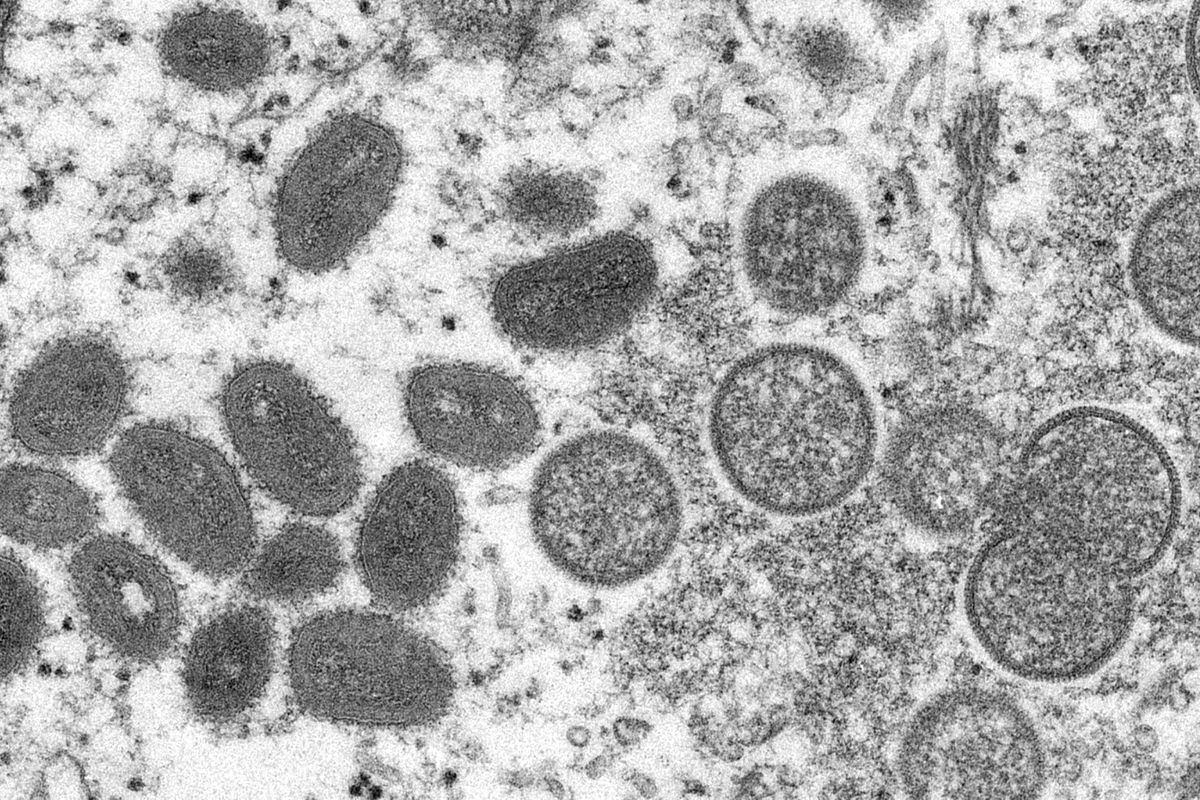
Monkeypox belongs to a family of viruses called smallpoxviruses. These can survive in bedding, clothing, and on surfaces, especially in dark, cool, low-humidity environments, according to the US Centers for Disease Control and Prevention. It notes on its website that a study found live viruses in a patient’s home 15 days after it was left uninhabited.
But the mere presence of the virus doesn’t mean it actually infects anyone.
Stephen Hoption Cann, a clinical professor at the University of British Columbia’s School of Population and Public Health, advised not to think about monkeypox in the same way as COVID-19.
Unlike COVID-19, people cannot get the virus at a grocery store, at a restaurant, or through shared transportation. “You’re not really going to catch this disease that way,” added Dr. Hoption Cann added.
How easy is it to spread?
Infectious disease specialist Allison McGeer said people cannot get monkeypox through accidental contact with contaminated objects, such as B. trying on clothes in a store, or insufficiently washed bed linen in a holiday home.
Before this current outbreak, data from African countries — where monkeypox is endemic — showed the virus wasn’t very transmissible, Dr. McGeer, a member of the Consortium on Emerging and Pandemic Infections and a professor in the Temerty Faculty of Medicine at the University of Toronto.
The spread of the virus has almost always taken place in homes and occasionally in hospitals, where there is close contact with patients’ skin and mostly when patients have had a serious illness with many skin lesions, she said.
How long does a person remain contagious?
People are thought to be contagious for about two to four weeks, from the onset of symptoms until their skin has completely healed and any scabs have fallen off their lesions or rashes, said Dr. Hope Cann.
It’s difficult to determine whether people without symptoms can transmit the virus because people could unknowingly pass it on if they have a lesion in the mouth or genital area where it may not be obvious, he said.
He added The cases that are occurring now can cause only one lesion, while patients in photos can have hundreds.
Ideally, people should be isolated while they are infectious, but he said if they have to go public they should cover any area that has a rash or lesion.
Who should get tested?
The main focus for testing and vaccinations is on gay, bisexual and other men who have sex with men, since most infections currently belong to this demographic, Dr. Hope Cann. People who have had multiple sex partners, don’t use condoms, or have a lot of intimate contact with others should get tested or vaccinated, he said.
dr However, Hoption Cann also noted the spread of the disease outside of this demographic.
Globally, monkeypox has been reported in some women and children in countries where the virus has never been seen before, although it still accounts for a small proportion of cases. (In Canada, 99 percent of cases are in men and the median age is 36, Canada’s Chief Public Health Officer Theresa Tam told reporters last week.)
Canadians can get tested for monkeypox based on a number of factors, including signs and symptoms of the disease or exposure to a case, according to the Public Health Agency of Canada. Because monkeypox can look similar to chickenpox or sexually transmitted infections like herpes and gonorrhea, people are advised to consult a healthcare provider and get tested.
Provinces and territories maintain individual websites with testing and vaccination information.
How long does it take for the monkeypox vaccine to start working?
This is still unknown. There are many questions about the timing and protection of the vaccines because the vaccines now used for monkeypox were developed for smallpox, said Dr. McGeer.
Although monkeypox vaccines were being tested, those tests were being conducted at a time when not enough of the disease was circulating for studies of vaccine effectiveness, she said. Animal experiments and immunogenicity studies, which measure immune responses in humans, show that the monkeypox vaccines are effective, she added. And there is evidence that people benefit from a single dose.
“But we really don’t know how effective these vaccines are,” she said.
BC releases details on monkeypox vaccine availability as outbreak spreads worldwide
How much protection does someone have from monkeypox if they were vaccinated against smallpox decades ago?
This too is unknown. According to the New York State Department of Health and Human Services, smallpox vaccination provides complete immunity for three to five years, after which immunity declines.
At this stage, it’s hard to tell how much immune protection Canadians who received a smallpox vaccine now have against monkeypox, said Dr. Hope Cann. Canada stopped routine smallpox vaccination in 1972.
“If a person was at high risk, I wouldn’t rely on the vaccine they received so many decades ago to protect them,” he said.
Written by Globe editors, our Morning Update and Evening Update newsletters give you a concise summary of the day’s most important headlines. Sign up today.
#Monkeypox #Outbreak #Explained #Symptoms #Vaccines #Spread

Leave a Comment