Like the roadrunner who outwits Wile E. Coyote, SARS-CoV-2 (the infectious virus responsible for COVID-19) is constantly mutating, creating new variants that can evade a well-trained immune system or a targeted drug vaccination.
Now scientists at Stanford Medicine have found a way to endow immune molecules once thought useless with the ability to put SARS-CoV-2 in a therapeutic headlock from which it can’t wriggle. Their method is described in an article published on September 8th natural chemical biology. The study was led by biologist and vaccine researcher Peter Kim, Ph.D.
Two things stand out about the study. First, while it’s not yet ready for human use, it’s a solid step toward developing broad-spectrum drugs that won’t stop working just because a nasty virus thinks up a new trick. And second, a key component of the new therapy was a molecule that was routinely thrown in the trash.
To fully appreciate Kim’s team’s discovery, let’s take a step back and ask: What exactly happens when a virus infects our bodies? And what does the immune system do about it?
The Basics of Infection
To cause an infection, a virus must first get into a cell. The outer membranes of cells are usually difficult to penetrate without a special pass. But these little vaultcrackers have figured out how to pick a lock on the cell’s surface, climb inside, hijack the cell’s replication machinery, make a bazillion copies of itself, and break out to spread to other cells.
The lock that SARS-CoV-2 knows how to pick is ACE2, which appears on the surface of cells in the throat, lungs, heart, kidneys, intestines and linings of blood vessels. Among other things, ACE2 is known for keeping our blood pressure low. But SARS-CoV-2 doesn’t care what ACE2 does for a living. Any cell that carries ACE2 is susceptible to SARS-CoV-2 infection.
Our immune system has ways of dealing with such invaders. Upon detecting the presence of a pathogen, B cells, which make up our immune system, pump out a wide array of antibodies directed against the invader. These are molecules that are uniquely suited to glowing onto pathogens like matching jigsaw puzzle pieces and—if glowing in exactly the right places and the fit is good—putting them out of action.
Antibodies that are excellent at latching onto a trait that is critical to the success of cellular safecracking of the pathogen are termed “neutralizing”: they prevent the pathogen from infecting cells. The best of these neutralizing antibodies can then be made into drugs.
For example, patients hospitalized with COVID-19 are often dosed with monoclonal antibodies: multiple copies of the same strong neutralizing antibody. The problem is that SARS-CoV-2 is adept at changing the shapes of its susceptible features through mutation, so that a monoclonal antibody, once neutralizing, loses its footing and can no longer suppress the new variant. The COVID-19 pandemic has been parade of one immune escape artist after another.
Souped Antibody
“It’s a slap in the face,” said Kim, who has spent much of his career in the pharmaceutical industry. “They go to all the trouble of developing these monoclonal antibodies, taking them through clinical trials, setting up manufacturing facilities, and getting emergency use authorization from the FDA. Then, months later, the virus mutates and the monoclonal antibody is no longer good.”
Of the more than half a dozen SARS-CoV-2-targeted monoclonal antibodies that have received emergency use authorization, only one is still in use.
But Kim’s lab has a souped-up antibody that can take on them all.
All monoclonal antibodies approved by the FDA to date attach to the receptor-binding domain (RBD) of SARS-CoV-2. This is the “end of business” for the virus’s infamous spike protein, the viral protrusion that plays around with ACE2 to gain access to cells. By shedding new variants with mutated RBDs, the virus shrugs off the access of successive monoclonal antibodies.
But the SARS-CoV-2 spike protein contains other regions that are, for all practical purposes, immutable. These regions are said to be highly conserved in evolutionary terms, meaning that they have not changed over time, even in virus strains that are different elsewhere.
So why not develop a monoclonal antibody that targets one of these conserved regions? Wouldn’t that solve the escape artist problem?
Yes, said Kim, who is a Virginia and DK Ludwig Professor of Biochemistry. “But so far no one has found an antibody against a conserved region on SARS-CoV-2 that is not a wimp.” In other words, it appears that none of these antibodies are strong neutralizing antibodies — they keep glowing and just sit there, riding carry with the virus but do not prevent it from infecting cells.
Wimp no more
Kim credits Payton Weidenbacher, Ph.D., a former graduate student in his lab, with a brainwave that sparked the advent of something called “ReconnAbs” (short for “receptor-blocking conserved non-neutralizing antibodies”). .
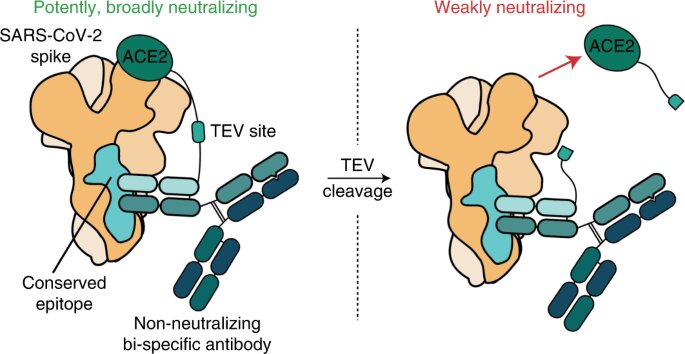
Weidenbacher’s idea: take another molecule that could neutralize SARS-CoV-2 and attach it to one of these weak but clingy antibodies, which binds to a well-conserved site on the viral spike protein.
“Many other researchers simply threw these antibodies in the trash can, and so did we,” says Weidenbacher.
They found an antibody that targeted a part of the SARS-CoV2 spike protein that never seems to change no matter what new variant emerges. Using a flexible piece of protein as a tether, they attached this antibody to the piece of ACE2 that protrudes from the cell surface – the part where the virus attaches itself.
“There is no way SARS-CoV-2 can mutate out of its dependency on ACE2,” said Weidenbacher.
In a laboratory dish, the tethered construct proved able to block SARS-CoV-2 infection of human cells that are normally susceptible to the virus. It worked on all SARS-CoV-2 strains tested up to BA.2.
The next step is to test ReconnAbs on animals.
Looking beyond the current pandemic, Kim envisions ReconnAbs serving as a modular, mix-and-match “parts kit” that could be deployed quickly when the next pandemic hits to stop the virus from getting started while what is hoped for is waiting for the development of even better medicines.
Such a kit would contain three parts: antibodies known to adhere tightly to highly conserved regions of any well-studied virus (e.g., a coronavirus or influenza virus); Whatever cell surface “lock” this virus knows how to pick to enter our cells; and small lines to hook them together.
“It was a creative blow,” Kim said. “Payton figuratively reached into the trash can, pulled out these lemons and turned them into lemonade.”
Powerful new antibody neutralizes all known SARS-CoV-2 variants
Payton A.-B. Weidenbacher et al, Conversion of non-neutralizing SARS-CoV-2 antibodies into broad-spectrum inhibitors, natural chemical biology (2022). DOI: 10.1038/s41589-022-01140-1
Provided by Stanford University
Citation: Molecular makeover makes wimpy antibody a SARS-CoV-2 attacker (2022 September 9) retrieved September 9, 2022 from https://phys.org/news/2022-09-molecular-makeover-wimpy- antibody-sars-cov-.html
This document is protected by copyright. Except for fair trade for the purpose of private study or research, no part may be reproduced without written permission. The content is for informational purposes only.
#Molecular #makeover #turns #weak #antibody #SARSCoV2 #attacker

Leave a Comment