Epidemic burden of hepatitis B in China
In parallel with the increase in HBV immunization rates, of which infant immunization rates reached 99.5% and timely birth dose immunization rates reached 96%, the prevalence of all chronic HBV infections (including CHB cases) is down 33.9 compared to 1992 % decreased in 2020 (70.83 million, almost 5.02% prevalence). By 2020, there were 26.77 million CHB cases, of which 11.66 million were undetected and 15.10 million were detected CHB cases, with the real-time detected rate of CHB cases increasing to 56%. Compared to 2020, the model predicted that the prevalence of total chronic HBV infections would increase to 55.73 million (3.95% prevalence) with a 48.0% decrease and the total number of CHB cases to 23.58 million with a decline of 12.0% in 2030 (Fig. 1A).
Estimated burden of chronic hepatitis B infection in China. A The number of chronic HBV infections and cases of chronic hepatitis B (CHB); B The estimated proportion of mother-to-child transmission accounts for the total number of chronic HBV infections; C the number of chronic HBV infections less than 5 years old. Note: Chronic HBV infection is defined as a dynamic process with HBsAg and/or HBV DNA positivity for more than 6 months, reflecting the interaction between HBV replication and the host immune response; while CHB is defined as a chronic inflammatory disease of the liver caused by persistent HBV infection. HBV Hepatitis B virus
In addition, the maximum proportion of cases with chronic HBV infection through mother-to-child transmission in the total number of chronic HBV infections is 25.6%. As predicted, it will decrease to approximately 10.92 million by 2030, accounting for 20.0% of the total number of chronic HBV infections, which has decreased by 31.1% compared to 2020 (Fig. 1B). As shown in Fig. 1C, the main beneficiaries of the infant vaccination strategy are newborns and children: compared to 1990, the prevalence of all chronic HBV infections in persons under 5 years of age has decreased by 98.6% in 2020 (0.16 million , 0.20% frequency).
The feasibility of WHO 2030 elimination targets
Due to the vaccination strategies initiated by health institutions and the Chinese government, the coverage of HBV vaccines in newborns has been greatly increased; infant HBV vaccine coverage has increased from 30.0% in 1992 to 99.5% in 2018; HBV vaccine coverage of timely birth dose reached 96% in 2018 (Fig. 1A). Vaccine uptake has already reached the coverage target of the WHO 2030 Elimination Goals. In addition, the model predicted that, with continued high immunization coverage after 2020, the prevalence of chronic HBV infection under age 5 would further decrease to 0.13% by 2030 (Fig. 1C). In addition, we found that increasing antiviral treatment coverage in patients with chronic HBV infection of childbearing potential to 41% could decrease the prevalence of chronic HBV infection below 0.1% (Fig. 2). The results of possible vaccination strategies to meet the WHO 2030 target of a 90% incidence reduction are presented in Supplementary File 1: Appendix p. 10.
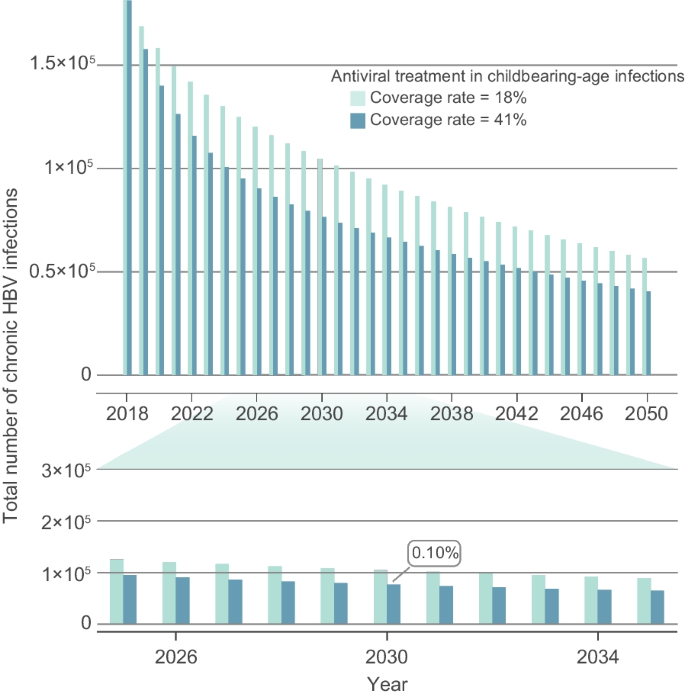
To explore strategies to achieve a prevalence of less than 0.1% in children under five by 2030. HBV hepatitis B virus, PMTCT Prevention of mother-to-child transmission
The impact of vaccination strategies against hepatitis B
The model results were compared across the four scenarios (see Methods). In the “status quo” scenario, the figure of 44.07 million chronic HBV infections (excluding CHB cases) in 2020 is estimated. The results showed that removal of all interventions (‘No intervention’ scenario) would have resulted in 78.21 million chronic HBV infections (excluding CHB cases) and almost 77.5% increase from the status quo by 2020. A Holding interventions constant with the No NIP and With NIP scenarios would result in 99.40 million and 82.67 million chronic HBV infections, 40.3% and 16.7% increases, respectively, from the status quo up to 2020. The total number of CHB cases in the No-Intervention Scenario, the No-NIP Scenario, and the With NIP Scenario would have increased to 41.32 million, 35.19 million, and 30.17 million, respectively, in 2020; However, the total number of CHB cases was 26.27 million in the status quo scenario as shown in Fig. 3A,B. Based on the model in the status quo scenario, 217.6 million people avoided contracting HBV as a result of hepatitis B immunization strategies in the past 30 years, while in the retained scenarios with the No NIP and the With NIP” (lower HBV vaccination rates than status quo scenario) only 70 million and 172.6 million people with HBV infection were avoided, (Fig. 3C).
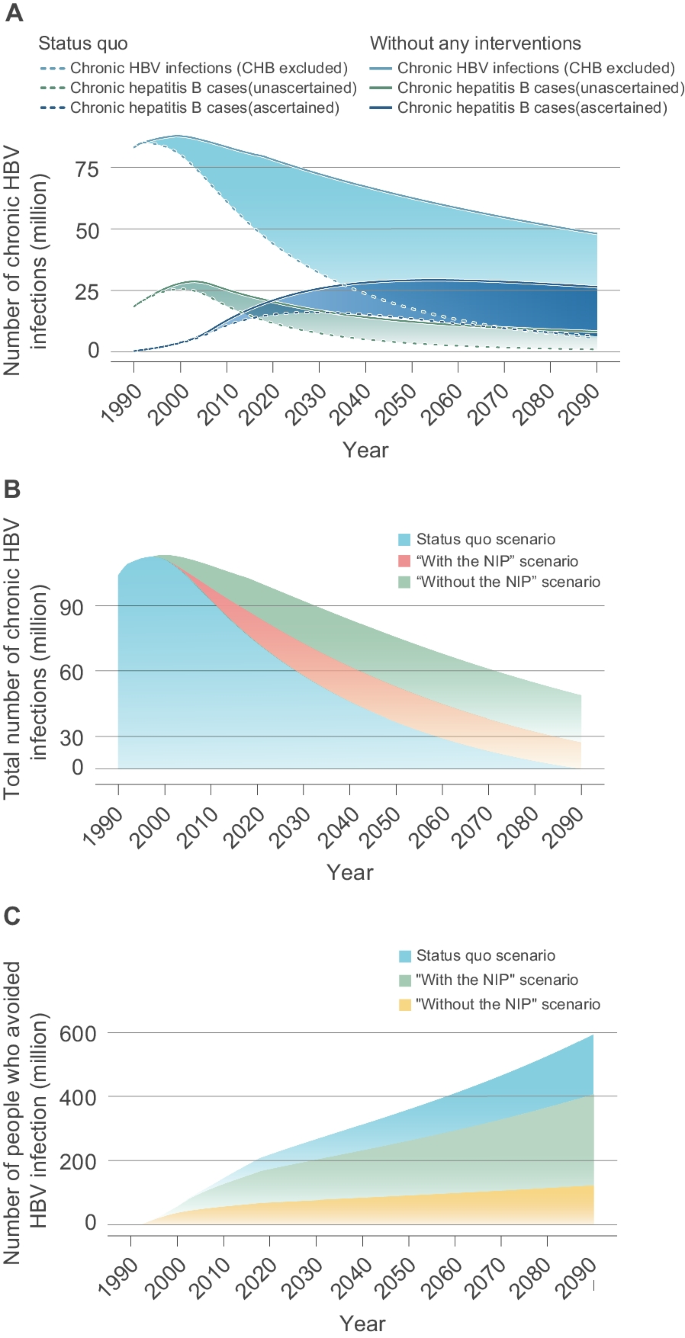
Effect of vaccination measures on the hepatitis B epidemic in China. A The prevalence of chronic HBV infection and chronic hepatitis B (CHB) cases in the status quo and no intervention scenarios, respectively. B The overall prevalence of chronic HBV infection containing CHB in the ‘Status quo’, ‘With NIP’ and ‘Without NIP’ scenarios. C The number of people who avoided HBV infection. See the Method section for more information on the definitions of these four scenarios. HBV Hepatitis B virus
Chronic HBV infections through mother-to-child transmission have declined significantly in response to interventions over the past 30 years. The number of chronic HBV infections infected via the mother-to-child route of transmission decreased from a projected 55.43 million in the scenario where all vaccination strategies were removed to 39.82 million when vaccination strategies included the No NIP” maintained, to 26.18 million if vaccination strategies maintained with “No NIP” scenario to 15.84 million in status quo in 2020 (Fig. 4A). In addition, 3.69 million chronic HBV infections would be added in 2020 if antiviral treatments and immunoglobulin interventions were removed from the PMTCT strategy (Fig. 4B).
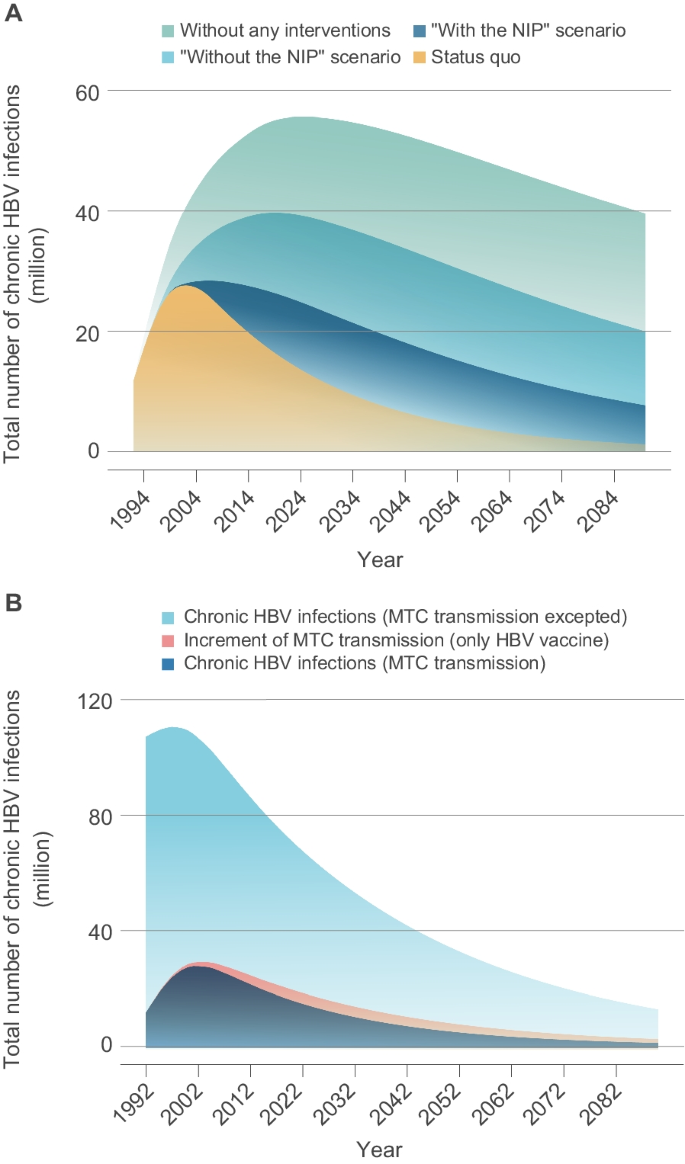
Effect of vaccination against hepatitis B on mother-to-child transmission. A The overall prevalence of chronic HBV infection by mother-to-child transmission (MTC) in the Status Quo Scenario, With NIP Scenario, Without NIP Scenario and in the No Intervention Scenario. B The overall prevalence of chronic HBV infection (light blue area) or chronic HBV infection tMTC transmission (blue area) in the “status quo” scenario; the “pink area” showed the increase in chronic HBV infections due to MTC transmission. HBV
hepatitis B virus, NIP
National Vaccination Program
economic forecasts
The model was run with cycle lengths ranging from one year to the average Chinese life expectancy (ie, from birth to age 77) to cover the lifelong experiences of the vast majority of newborns. The cost-benefit analysis in Table 1 showed that the total cost per capita with the current infant immunization strategy in the “status quo” scenario is US$1260.78, while the “no intervention” scenario costs per capita of $1260.78 had $13,177.03. Implementation of the infant immunization strategy increased vaccination costs by $52.17 but reduced costs associated with HBV infection by $11,968.42 for a net benefit of $11,916.25. In the “status quo” scenario, the PMTCT strategy demonstrated a net benefit of $11,283 per person, with a BCR of 12.66, which was higher than that of the infant vaccination strategy at 9.49. Out of 10.03 million newborns born in China in 2020, a total of 0.52 billion were needed to implement the infant vaccination strategy, generating a benefit of about 120.10 billion.
The cost-effectiveness analysis showed that implementation of the infant immunization strategy and the PMTCT strategy in the status quo scenario can increase QALYs per person by 1.54 and 1.58, respectively. Compared to the no-intervention scenario, the former could save $7,737.82 for each QALY increase and the latter $7,726.03, suggesting that both are cost-effective intervention measures. Compared to the infant vaccination strategy, the cost of PMTCT decreased by $290.89 and the effect increased by 0.04 QALY, further reducing costs while reducing infant infections.
sensitivity analysis
According to the one-sided sensitivity analysis with the range of values shown in Supplementary File 1: Table S2, both the infant vaccination strategy and the PMTCT strategy strategies were cost-saving. Even when the vaccination rate was adjusted to 0.3, as was the case in 1992, the infant vaccination strategy still reduced the cost associated with HBV infection by $3794.98. The probabilistic sensitivity analysis in additional file 1: Fig. S8 showed that when the parameters were varied within the set value range, the ICER of the PMTCT strategy was always cost-saving compared to the infant vaccination strategy and the results were very stable. We continued to monitor the economic benefits of the two strategies by continuously reducing the prenatal screening rate and the HBIG coverage rate. Figure 5 showed that when both parameters decreased by 30% compared to PMTCT, the infant vaccination strategy was more cost-effective even at a WTP (willingness-to-pay) equal to simple GDP per capita.
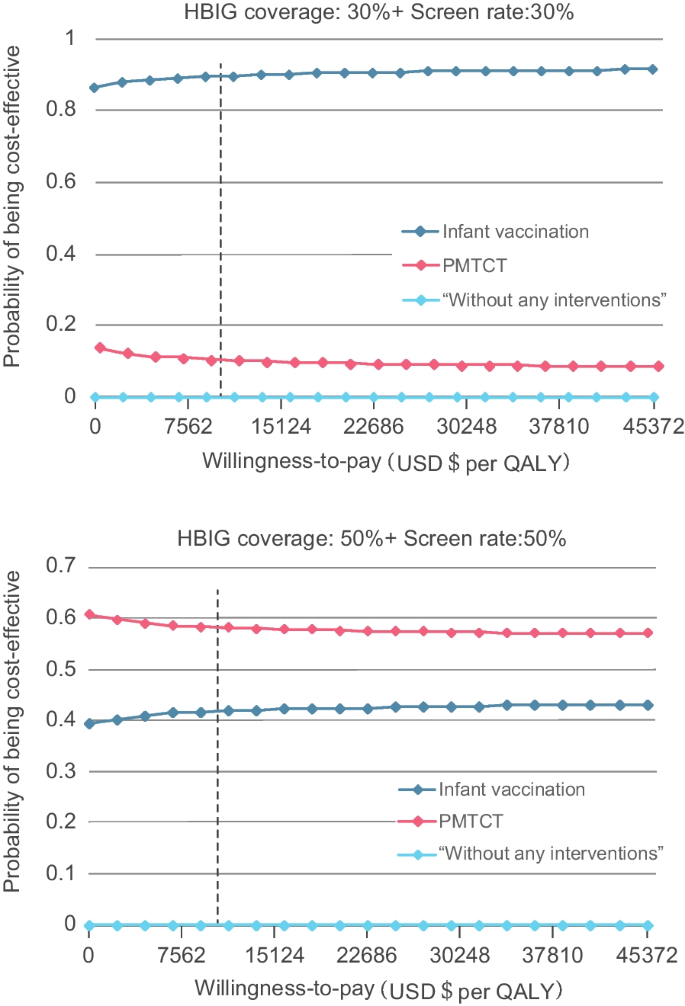
Cost-benefit-acceptance curves for vaccination strategies. Cost-effectiveness-acceptance curves of infant vaccination strategy (blue curve) and PMTCT strategy (red curve) under 50% and 30% HBIG coverage and screening rate. USD U.S. dollar, HBIG hepatitis B vaccination program, QALY quality-adjusted life year, PMTCT the prevention of mother-to-child transmission
#Impact #Chinas #national #hepatitis #immunization #program #modeling #study #infectious #diseases #poverty

Leave a Comment