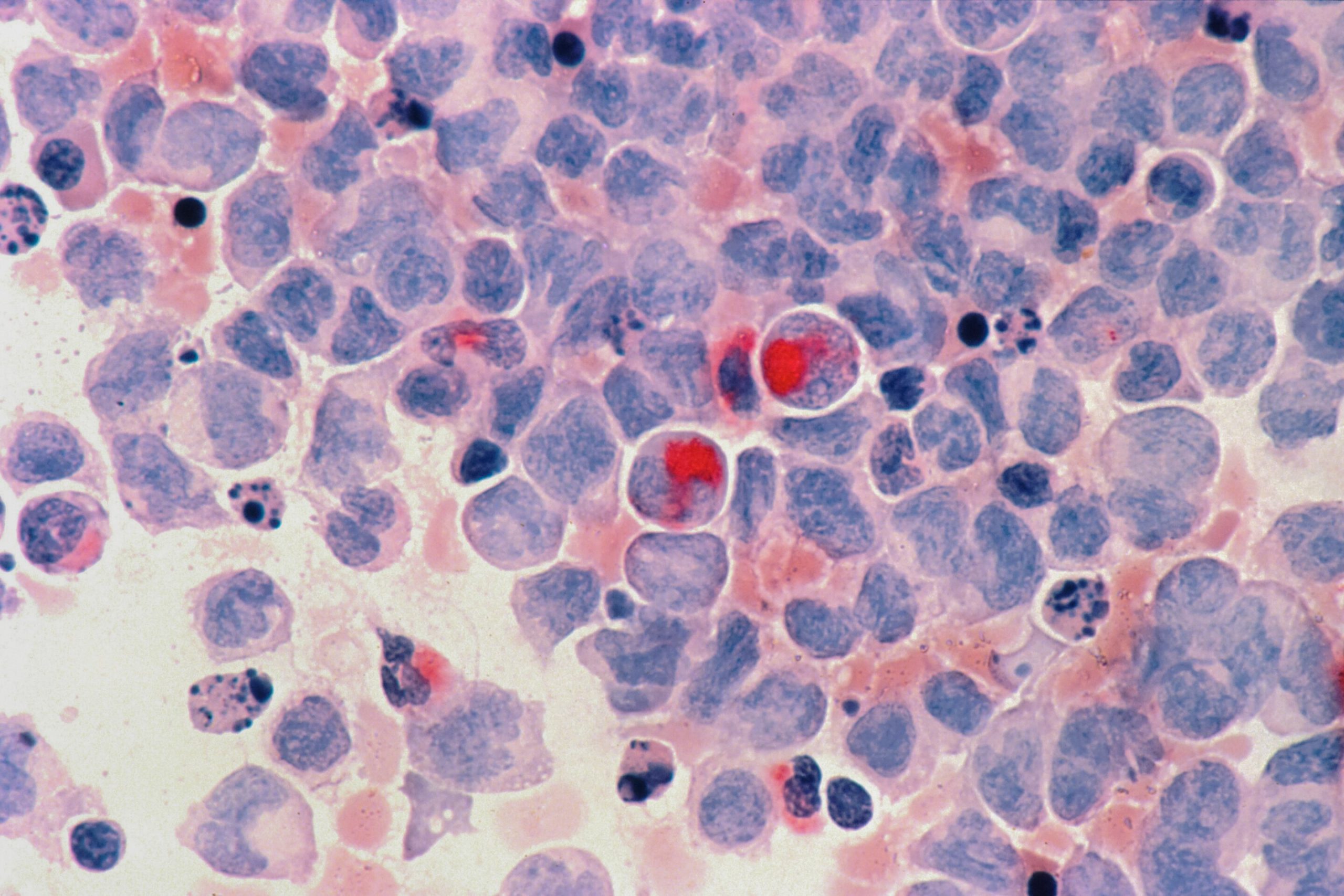
Photo Credit: Unsplash/CC0 Public Domain
The statistics for pancreatic cancer are sobering. With a five-year survival rate of just 9%, the incidence of the most common type, pancreatic ductal adenocarcinoma (PDAC), is increasing and is projected to be the second leading cause of cancer deaths by 2030. Surgery remains the most effective treatment to date In 70-80% of patients, surgery is not a viable option. Understanding pancreatic cancer at the cellular and subcellular levels is critical to developing therapies that can buy patients more time.
One way to prolong survival is to optimize the treatment strategy and switch strategies promptly if treatment is not effective. Treatments can include a mix of radiation and chemotherapy. Currently, assessing how well PDAC patients are responding to this therapy typically relies on imaging and measuring blood serum levels of cancer biomarkers. However, both of these methods have disadvantages. Imaging (CT, MRI) cannot detect small tumors or distinguish benign from malignant, while the best-established PDAC marker is absent in 5-20% of PDAC patients and can provide unreliable results.
From Garbage to Gold
A study published today in cells from the Systems Oncology Lab at Champalimaud Research offers a potential turning point in assessing treatment response in PDAC patients.
Bruno Costa-Silva, lead researcher and lead author of the study, first explored the potential of so-called “extracellular vesicles” (EVs) in fighting cancer in 2008. “EVs are tiny sacs released by cells. They are like mini cells with a lipid membrane, genetic material, proteins and sugars. For a long time they were thought to be “garbage bags” filled with waste products that cells wanted to dispose of. But it is now clear that they also transmit messages between cells.”
Since plants and bacteria also release these small vesicles, electric vehicles could be one of the strongest forms of communication in living organisms. They are produced by virtually all cells, including cancer cells. In fact, studies show that EVs secreted by malignant and non-malignant cells can significantly contribute to tumor progression.
In previous studies, Costa-Silva found that EVs in the blood could be used to detect, predict and localize pancreatic cancer metastases. So far, however, researchers have used one-time measurements of EVs in patients for either prognosis or diagnosis. “Our study is the first to show that we can use the change in electric vehicle use in pancreatic cancer patients over time to determine how well they respond to therapy,” says Costa-Silva.
From idea to discovery
When Nuno Couto, an oncologist at the Champalimaud Foundation and lead author of the study, began investigating the potential of electric vehicles to monitor treatment response, the team found a surprising result. “At first we thought it was an artifact,” says Couto. “But it quickly became clear that EVs in PDAC patients had significantly higher levels of a particular protein compared to EVs in healthy controls.” Finds and kills cancer cells.
“The next step was the most difficult,” admits Couto. “To see how the levels of these IgG-positive EVs change in patients over the course of treatment, we had to draw 20-30 blood samples from the same patient over many months. Without the help of the patients, nurses, clinicians, and pathologists at the Champalimaud Clinical Center, this study simply would not have been possible.”
Using a special method developed by Costa-Silva’s laboratory to quickly measure EV populations in tiny blood samples, the team found that IgG-positive EVs increase during disease progression and decrease in response to therapy . As a result, these EVs represent a new biomarker that expands the repertoire of available tools to assess tumor status, particularly for the many patients who do not express the current standard biomarker and for whom imaging is the only indicator of treatment response .
“We were very excited to see such a close correlation between these vesicles and response to therapy,” says Costa-Silva. “We now have a more reliable tool to assess and improve the effectiveness of PDAC treatments and be more ineffective in reducing the unnecessary and harmful side effects.”
From oncology to cell biology
“This finding prompted me to change the orientation of my laboratory,” assures Costa-Silva. “It’s impossible to look at these results and not think about the immunology or the broader implications for cell signaling.”
The researchers found that IgG binds to electric vehicles via a known cancer antigen in PDAC patients. They hypothesize that EVs expressing this antigen are released from the cancer itself, so IgGs become attached to the EVs rather than their intended target: the tumor cells. That way, the tumor would be able to evade the immune system’s arsenal and launch electric vehicles to intercept IgG missiles.
“If very aggressive cancers like PDAC use EVs to disarm the immune system, we can develop new therapies that target tumor-derived EVs and make these cancers less treatment-resistant,” notes Costa-Silva. His team is now investigating whether proteins expressed by EVs in other types of cancer also interact with molecules of the immune system.
As Costa-Silva puts it, “This is really about cell physiology. Crayfish can use EVs to disrupt immunity, but EVs also serve important functions in noncancerous environments. Once released from a cell, proteins on the surface of EVs interact with other proteins and regulate their ability to interact with cellular targets, causing a cascade of sequelae in other cells. We are very interested in learning more about these post-secretory interactions and how EVs act as regulators of cell signaling.”
“There’s still so much we don’t know about how cells communicate with each other,” adds Costa-Silva. “If we can understand the language of cells and decode how electric vehicles regulate the activity of molecules involved in physiological and pathological processes, we can use this knowledge to address a wide range of problems, from autoimmune diseases to age-related disorders . That’s just the beginning.”
Scientists discover molecule that kills pancreatic cancer cells
More information:
IgG+ extracellular vesicles measure therapeutic response in advanced pancreatic cancer, cells (2022).
Provided by the Champalimaud Center for the Unknown
Citation: Researchers Discover New Tool to Improve Pancreatic Cancer Care (2022 September 8) Retrieved September 10, 2022 from https://medicalxpress.com/news/2022-09-tool-pancreatic-cancer.html
This document is protected by copyright. Except for fair trade for the purpose of private study or research, no part may be reproduced without written permission. The content is for informational purposes only.
#Researchers #discover #tool #improve #treatment #pancreatic #cancer

Leave a Comment