The American College of Chest Physicians has issued an updated clinical practice guideline for the perioperative management of antithrombotic therapy published in chest.
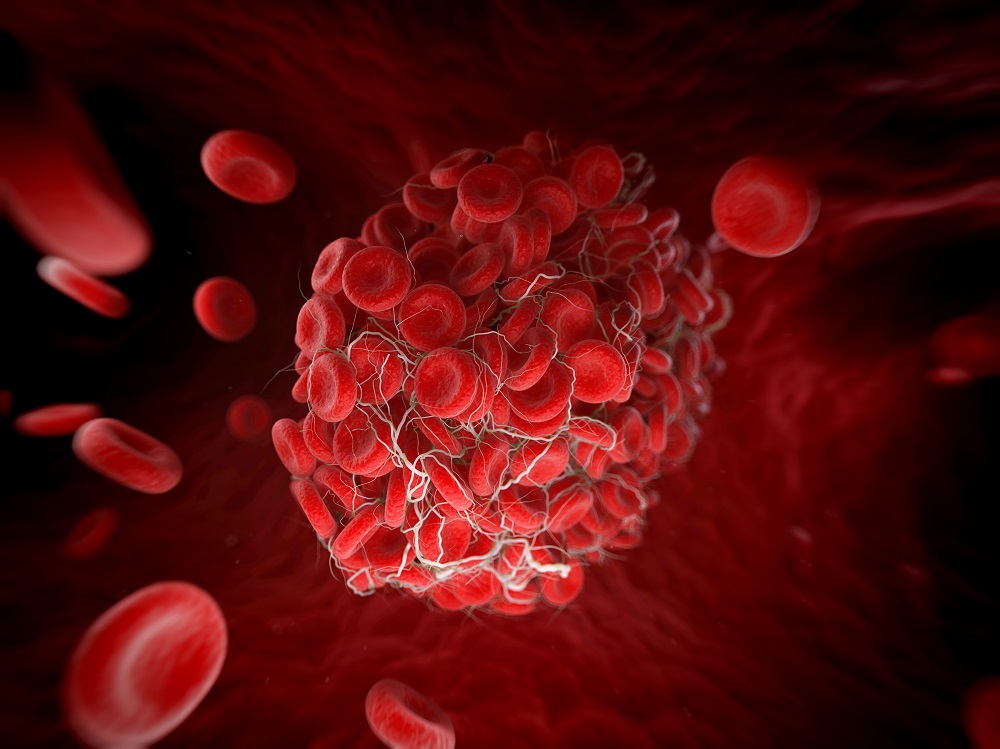
More than 10 million people are evaluated annually worldwide for the management of perioperative antithrombotic therapy; Such therapy includes vitamin K antagonists (VKA), direct oral anticoagulants (DOAC), heparin bypass, and antiplatelet drugs for those who require surgery or an invasive procedure. The goal of perioperative antithrombotic management is individualized, patient-centered care and minimization of perioperative thromboembolism and bleeding.
The new guideline, which addresses 43 Patient-Intervention-Comparator-Outcome (PICO) questions, is a significant update to the 2012 guidelines, which addressed 11 PICO questions. The new guideline also contains 44 evidence-based recommendations on the PICO questions. New topics in the guideline include the perioperative management of patients receiving direct oral anticoagulants (DOACs) and P2Y12 Inhibitors of antiplatelet agents and guidance on perioperative laboratory testing.
Continue reading
“The target audience of this guideline is the broad spectrum of clinicians involved in perioperative patient care, but it is also relevant for researchers to identify areas for future study, for patients to access a reliable source of information, and for clinical managers to facilitate the development of standardized patient care pathways,” the authors said.
A focus on 4 patient groups
The PICO questions and guideline statements are grouped into 4 categories reflecting the 4 patient groups that clinicians typically face: (1) patients receiving a vitamin K antagonist (VKA) focused on warfarin; (2) patients receiving a VKA and using perioperative bypass with heparin; (3) patients receiving a DOAC; and (4) patients receiving an antiplatelet agent. The PICO questions are also designed to address numerous practical aspects of perioperative antithrombotic therapy management.
The guideline followed the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach. A recommendation for each PICO question was rated as strong (“we recommend”) or conditional (“we recommend”). The certainty of the evidence was categorized as high, moderate, low, or very low.
Heparin bridging, VKA therapy and cardiac interventions
The guideline authors made 2 strong recommendations with moderate evidence. The first strong recommendation is against the use of heparin bridging in patients receiving VKA therapy for atrial fibrillation who require VKA interruption for elective surgery or intervention. The second strong recommendation is to continue VKA vs. VKA interruption and heparin bypass in patients receiving VKA therapy who require a pacemaker or internal cardiac defibrillator implant. The authors noted that the continuation of VKAs associated with cardiac device procedures is based on the premise that a patient’s international normalized ratio at the time of the procedure is less than 3.0.
The guideline authors describe 18 of their recommendations as “key recommendations”. Among other things, the authors suggest against the use of heparin bridging in patients receiving VKA therapy for a mechanical heart valve who require VKA disruption for elective surgery or surgery. The authors advise against the use of heparin bridging for patients who receive VKA therapy for venous thromboembolism as the only clinical indication and who require VKA interruption for elective surgery or intervention.
Therapy interruptions for other interventions
In patients on VKA therapy who require VKA interruption for colonoscopy with anticipated polypectomy, the authors advise against the use of heparin bridging during VKA interruption.
In patients receiving dabigatran who require elective surgery or surgery, the authors suggest stopping dabigatran 1 to 4 days before surgery or surgery rather than continuing dabigatran therapy.
For patients receiving edoxaban who require elective surgery or surgery, the authors suggest stopping edoxaban 1 to 2 days before surgery or surgery rather than continuing edoxaban.
The authors suggest that in patients receiving rivaroxaban who require elective surgery or surgery, rivaroxaban should be stopped 1 to 2 days prior to surgery or surgery rather than continuing rivaroxaban treatment.
Direct oral anticoagulants
The authors advise against the use of perioperative heparin bridging in patients who require DOAC disruption for elective surgery or intervention.
The guideline authors also suggest resuming DOAC more than 24 hours after surgery or intervention versus resuming DOAC within 24 hours in patients in whom DOAC was interrupted due to elective surgery or intervention. In patients in whom DOAC has been interrupted due to elective surgery or intervention, the authors advise against routine DOAC coagulation function testing to guide perioperative DOAC management.
acetylsalicylic acid
In patients receiving ASA and undergoing elective non-cardiac surgery, continuation of acetylsalicylic acid (ASA) treatment is recommended versus discontinuing ASA treatment. For patients receiving ASA who are undergoing coronary artery bypass graft surgery, the authors suggest continuing ASA rather than interrupting it. In patients receiving a P2Y12 Inhibitor drug, the authors suggest interrupting the P2Y12 Inhibitor versus continuation perioperatively.
Platelet aggregation inhibitors, P2Y12 Inhibitors
In patients receiving antiplatelet drug therapy and undergoing elective surgery or surgery, the authors advise against the routine use of platelet function tests prior to surgery or surgery to guide perioperative platelet aggregation management. In patients receiving ASA and a P2Y12 inhibitor who have had coronary stenting within the past 3 to 12 months and are undergoing elective surgery or procedure, the authors suggest discontinuing P2Y12 Inhibitor before surgery vs. continuation of P2Y12 Inhibitor.
“Although there have been important advances in the perioperative treatment of anticoagulants and antiplatelet agents, much work remains to fill knowledge gaps,” the authors say. “A challenging area of research is the perioperative management of antiplatelet therapy, particularly in patients with coronary stenting receiving ASA and a P2Y12 Inhibitor because there are several factors (timing of stent placement, type of surgery, type of antiplatelet treatment) that make well-designed randomized trials difficult to conduct.”
guideline development process
The guideline panel consisted of a multidisciplinary group of clinicians, including internists, thrombosis specialists, cardiologists, anesthesiologists, surgeons, critical care physicians, and pharmacists, collaborating with methodologists from the Mayo Clinic Evidence Center.
The systematic review was conducted across multiple databases through July 2021 and was limited to English-language articles and human studies, and by article type (clinical study, randomized clinical trial, and systematic review).
references
Douketis JD, Spyropoulos AC, Murad MH, et al. Perioperative management of antithrombotic therapy: a clinical practice guideline from the American College of Chest Physicians. Chest. Published online August 9, 2022. doi:10.1016/j.chest.2022.07.025
Douketis JD, Spyropoulos AC, Murad MH, et al. Perioperative management of antithrombotic therapy: a summary of the American College of Chest Physicians clinical practice guideline. Chest. Published online August 10, 2022. doi:10.1016/j.chest.2022.08.004
#ACCP #updates #guideline #perioperative #management #antithrombotic #therapy

Leave a Comment