Image source: Constante M, Libertucci J, Galipeau HJ, et al. (in print). gastroenterology. 2022.
Celiac disease affects about 1% of the population, although a much higher percentage of the population carries the genetic risk factors and consumes gluten, the disease-causing factor. The gut microbiota is emerging as an important cofactorthis may help explain why some genetically predisposed people develop celiac disease and others do not. The only current treatment for celiac disease is a strict gluten-free diet for life, which is difficult to follow, expensive, and does not always result in complete resolution of symptoms and inflammation. A better understanding of the relatively unknown role of the small intestine microbiota in celiac disease could help us prevent or better treat existing diseases.
Research groups have made efforts to identify microbiota differences in cross-sectional studies of celiac disease patients compared to healthy controls and in longitudinal studies in which “at risk” individuals are followed until they develop celiac disease-specific antibodies. Similar to other chronic inflammatory diseases, the microbial changes associated with celiac disease vary between studies and are not always consistent between studies.
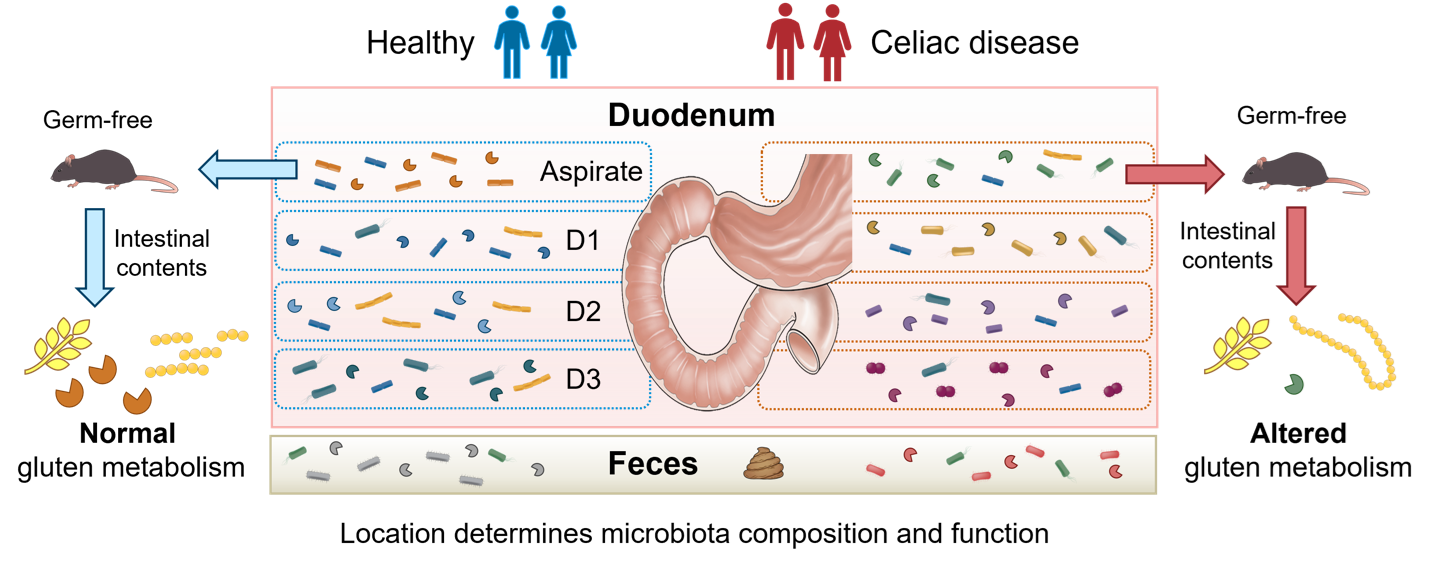
according to dr This is not surprising to Marco Constante of McMaster University (Hamilton, Canada); “To date, studies examining the gut microbiota in celiac disease have varied in design, sampling location, and control populations.” In addition, most studies have looked at the composition of the stool microbiota. “Inflammation in celiac disease occurs primarily in the upper small intestine, known as the duodenum, and microbial changes that occur in the feces may not reflect the changes that occur in the small intestine. This makes it difficult to gain insight into possible mechanisms at the site of the disease,” says Dr. constant.
A new study published in gastroenterology shows gastrointestinal situation a key determinant of microbiota composition and function in celiac disease.
The one from Dr. Alberto Caminero and Dr. The study, led by Elena Verdu of McMaster University, aimed to analyze the gut microbiota along the gastrointestinal tract in patients with active celiac disease compared to healthy individuals. They examined the microbial composition and function in biopsies from different sections of the duodenum as well as in small intestine aspirates and faeces.
Location along the gastrointestinal tract, rather than the presence or absence of celiac disease, was the strongest determinant of microbiota composition. However, microbial differences were actually found between celiac disease patients and controls that were specific to each site. Importantly, the microbiota composition in biopsies from the duodenum is clustered according to the severity of the inflammation. Neisseria, an opportunistic pathogen previously found to be more prevalent in patients with active celiac disease, was associated with more severe enteropathy.
Even in different sections of the duodenum, site-specific differences between patients with celiac disease and controls were observed, underscoring the importance of reporting the exact sampling site in studies. Duodenum-specific differences were also observed when function of the microbiota was analyzed and showed an altered microbial proteolytic function in patients with celiac disease.
It is known that proteases from bacteria can digest gluten, increasing or decreasing the immunogenicity of gluten. Indeed, microbial gluten-degrading enzymes such as novel computer-controlled endopeptidases and latiglutenase are currently being investigated in clinical trials with promising results for improving gluten-induced symptoms and consequent quality of life.
the constant et al. The study also examined mechanisms using germ-free mice colonized with small intestinal microbiota from celiac disease patients. These mice developed an impaired ability to digest gluten, in parallel with higher expression of immunogenic gluten peptides in the gut. The expression of microbial glutamate carboxypeptidase was lower in the duodenum of celiac disease patients, and its decrease in mice also correlated with impaired gluten breakdown, suggesting a potential candidate for future therapeutic development.
“This is one of the first studies to conduct a comprehensive comparison of the small intestine and fecal microbiota in celiac disease, allowing us to identify specific microbial niches in celiac disease,” says Dr. Caminero, assistant professor at McMaster University and co-director of the course. Stool is often used to study the composition of the microbiota in celiac disease because it can be easily obtained from study participants; However, the changes observed in the stool were not always observed in the small intestine. “The results of our study underscore that sampling location should be considered as a confounding factor when investigating the role of microbiota in celiac disease,” adds Dr. Verdu, a professor at McMaster University and corresponding author of the study.
References:
Verdu EF, Schuppan D. Cofactors, microbes, and immunogenetics in celiac disease as a guide to novel approaches to diagnosis and treatment. gastroenterology. 2021 Nov;161(5):1395-1411.e4. doi: 10.1053/j.gastro.2021.08.016. Epub August 17, 2021. PMID: 34416277.
Constante M, Libertucci J, Galipeau HJ, et al. (in print). gastroenterology. 2022.
Caminero A, Galipeau HJ, McCarville JL, Johnston CW, Bernier SP, Russell AK, Jury J, Herran AR, Casqueiro J, Tye-Din JA, Surette MG, Magarvey NA, Schuppan D, Verdu EF. Duodenal bacteria from patients with celiac disease and healthy subjects significantly influence gluten breakdown and immunogenicity. gastroenterology. 2016 Oct;151(4):670-83. doi: 10.1053/j.gastro.2016.06.041. Epub June 30, 2016. PMID: 27373514.
Pultz IS, Hill M, Vitanza JM, Wolf C, Saaby L, Liu T, Winkle P, Leffler DA. Gluten degradation, pharmacokinetics, safety and tolerability of TAK-062, a modified enzyme used to treat celiac disease. gastroenterology. 2021 Jul;161(1):81-93.e3. doi: 10.1053/j.gastro.2021.03.019. Epub March 17, 2021. PMID: 33741317.
Syage JA, Green PHR, Khosla C, Adelman DC, Sealey-Voyksner JA, Murray JA. Latiglutenase treatment in celiac disease: improvement of symptoms and quality of life in seropositive patients on a gluten-free diet. GastroHep. 2019 Nov;1(6):293-301. doi: 10.1002/ygh2.371. Epub 8 Oct 2019. PMID: 32313451; PMC ID: PMC7169937.
#Small #intestine #microbiome #littleunderstood #ecosystem #celiac #disease

Leave a Comment