October 17, 2022
2 minutes read
Source/Disclosures
Published by:
Disclosure:
Saw reports financial ties to Abbott, AstraZeneca, Baylis, Boston Scientific, FEops, St. Jude Medical, Dienst, Sunovion, and WL Gore and Associates. Persu does not report any relevant financial disclosures. The relevant financial information of all other authors can be found in the study and in the editorial.
In a large cohort of patients with spontaneous coronary artery dissection, mortality rates and the rate of recurrent spontaneous coronary artery dissection at 3 years were low, the researchers reported.
Most patients were not revascularized and many were treated with aspirin and/or beta-blockers, according to results published in Journal of the American College of Cardiology.

Data are from Saw J, et al. J Am Coll Cardiol. 2022;doi:10.1016/j.jacc.2022.08.759.
Jacqueline Saw, MD, interventional cardiologist at Vancouver General Hospital and St. Paul’s Hospital, program director of the Vancouver General Hospital Interventional Cardiology Fellowship Program and clinical assistant professor of medicine at the University of British Columbia and colleagues conducted a prospective study of 750 patients with spontaneous coronary artery dissection (SCAD ) enrolled at 22 North American centers between June 2014 and June 2018.
The mean age of the cohort was 52 years, 88.5% were women (55% postmenopausal), 31.3% with STEMI and 68.3% without STEMI. In addition, 50.3% had a triggering emotional stressor and 28.9% had a triggering physical stressor, while 42.9% had fibromuscular dysplasia, 4.5% were in a peripartum state, and 1.6% had a predisposing genetic disorder exhibited.
Most (84.3%) patients received conservative treatment, 14.1% had PCI and 0.7% had CABG, Saw and colleagues wrote.
death, recurrence rates
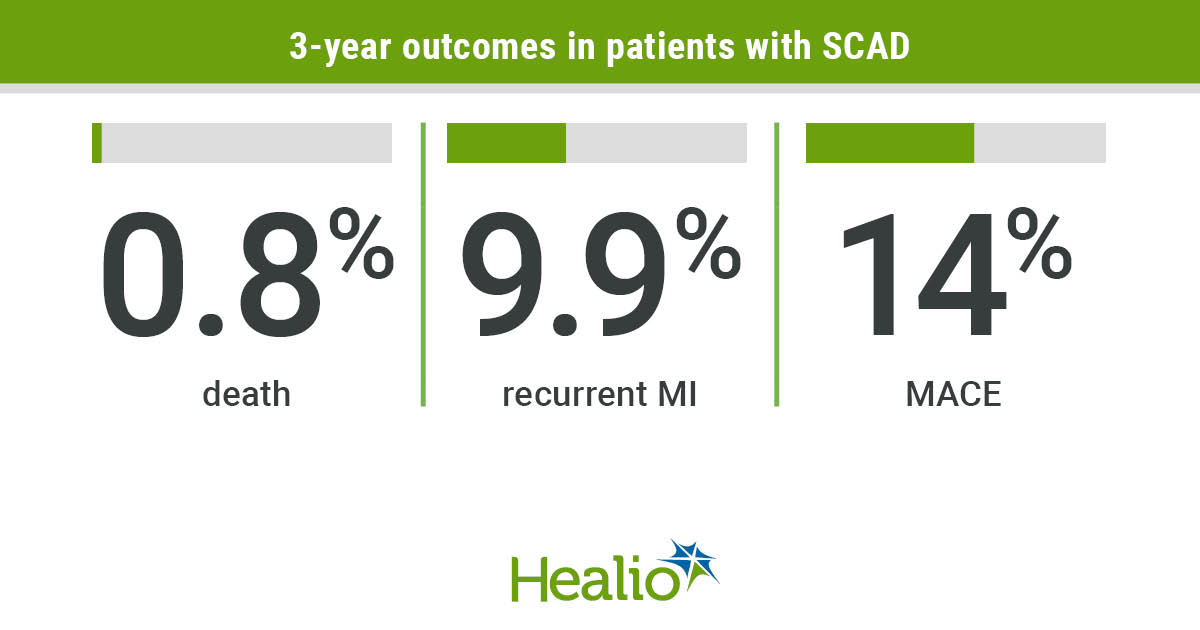
At a median follow-up of 3 years, 0.8% died, 14% experienced a major adverse cardiovascular event, and 9.9% had recurrent MI (3.5% with dilatation of prior SCAD, 2.4% with de novo recurrent SCAD and 1.9% with iatrogenic indication). dissection), according to the researchers.
Independent predictors of major adverse cardiovascular events at 3 years were the presence of a genetic disorder (HR = 5.05; P < 0.001), peripartum status (HR = 2.17; P = 0.027) and extracoronary fibromuscular dysplasia (HR = 1.51; P = 0.038).
Rates of major adverse cardiovascular events at 3 years did not differ between those who had PCI at Index hospitalization and those who did not, Saw and colleagues found.
At 3 years, 80% of patients were taking aspirin and 73.5% were taking beta-blockers, and medication use was not associated with the risk of serious cardiovascular adverse events, the researchers wrote.
“Our finding of low major major cardiovascular events and mortality up to 3 years is remarkably low compared to previous published reports,” Saw and colleagues wrote. “Previously, rates of major cardiovascular events of up to 30% with a follow-up of 2 to 3 years have been reported, mainly caused by recurrent myocardial infarction due to recurrent SCAD, reported in 15% to 22% of patients. … In our current large study, prospective recruitment of consecutive patients presenting to hospitals acutely with SCAD minimized patient selection bias and thereby provided a more accurate estimate of the natural history of SCAD.”
“Deserves a detailed analysis”
In a related editorial alexandre persMD, PhD, Head of the Hypertension Clinic, Department of Cardiology, Cliniques Universitaires Saint-Luc, Université Catholique de Louvain, Brussels, and colleagues wrote that the study “suggests a better prognosis and reduced SCAD recurrence rate in fewer selected, more representative SCAD patients. It merits close analysis by anyone interested in the diagnosis and care of patients with SCAD and provides further motivation for clinical trials of this disease.”
Relation:
#Mortality #recurrence #years #large #SCAD #cohort

Leave a Comment