It is a well-known fact that drinking large amounts of alcohol, even for just a few days, triggers fat accumulation in the liver and eventually leads to alcohol-related liver disease. On the other hand, if fat accumulates in the liver even without alcohol consumption, this is referred to as non-alcoholic fatty liver disease (NAFLD). NAFLD is a potentially serious chronic liver disease that affects approximately 25% of adults worldwide. Patients with NAFLD are 33% more likely to have coronary artery disease compared to healthy controls.
Despite being a severe and chronic liver disease closely associated with several other diseases, the underlying mechanisms associated with NAFLD remain more or less elusive. To this end, researchers from China recently conducted a meticulous literature review and produced an overview based on their findings. Your article was published in Chinese Medical Journal on July 06, 2022.
dr Chengfu Xu, corresponding author of the article and principal investigator at Zhejiang University School of Medicine, China, states: “In recent years, the prevalence of NAFLD-associated hepatocellular carcinoma has shown an increasing trend in many countries. The proportion of hepatocellular carcinomas attributed to NAFLD has tripled in Korea from 3.8% in 2001-2005 to 12.2% in 2006-2010. This proportion increased in France from 2.6% in 1995-1999 to 19.5% in 2010-2014. As such, NAFLD represents a significant drain on global health resources and the economy.”
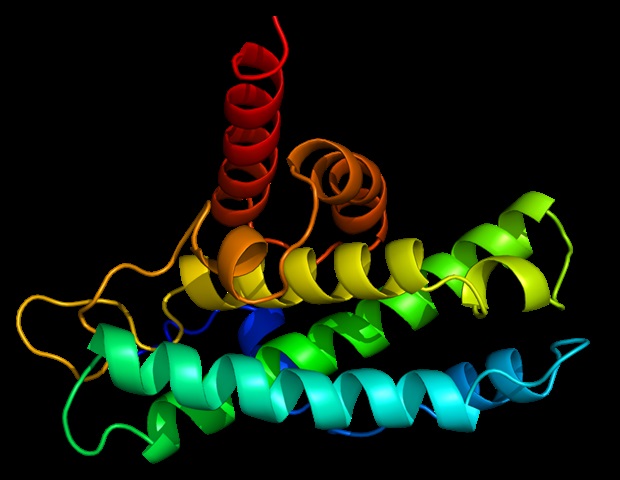
Retinol, or vitamin A, is a fat-soluble vitamin that is primarily stored in the liver and transported to other organs by binding to retinol-binding protein 4 (RBP4). In the target organs (e.g. eyes), retinol can be taken up by binding of RBP4 to cell membrane receptors. However, the role of RBP4 in the development of insulin resistance and obesity has received much attention only recently.
Although several observational studies have also shown the association of serum RBP4 with NAFLD risks, the results have revealed several apparent contradictions. New clinical studies draw attention to the role of RBP4 in NAFLD. In the review article, the researchers provided a global overview of the RBP4 landscape and highlighted the latest findings of clinical importance.
In the overview, the authors cite several studies that are relevant to the problem under investigation. For example, they cite a 2005 paper in which researchers reported the association between elevated serum RBP4 levels and insulin resistance. dr Xu and his colleague also cite conflicting research. For example, although a Turkish study reported higher serum RBP4 levels in obese children suffering from NAFLD, an Italian study found a negative correlation between serum RBP4 levels and NAFLD activity score in pediatric patients with NAFLD.
dr Xu explains “These conflicting results may result from the heterogeneity of the methods used to detect fatty liver and the race of the study participants, as well as from the limited size of the study sample. The studies that did not observe a significant association or inverse association between RBP4 levels and NAFLD all diagnosed fatty liver by biopsy. Liver biopsy represents the gold standard for diagnosing NAFLD. It is worth noting that none of these studies found a significant correlation between the RBP4 serum levels and fasting body mass index, waist circumference, and plasma glucose or insulin levels were found, although the correlation has been confirmed in a number of studies.”
The review also sheds light on some of the physiological mechanisms involved. For example, it is known that free RBP4 can be easily filtered in the kidneys due to its low molecular weight. However, transthyretin (TTR), a thyroid hormone carrier, binds RBP4 and prevents it from being filtered. However, a therapeutic drug called fenretinide dissociates RBP4 from TTR, thereby facilitating the renal excretion of RBP4, lowering circulating RBP4 levels in the process.
“First, clinical observations have found that circulating RBP4 levels are closely associated with NAFLD risk, but discrepancies still exist. Second, fundamental studies have confirmed that RBP4 is involved in the pathogenesis of NAFLD by inducing de novo hepatic lipogenesis, impairing fatty acid oxidation, exaggerating insulin resistance and promoting inflammation. Third, drugs aimed at reducing circulating RBP4 levels and downregulating hepatic RBP4 expression showed protective effects against NAFLD. These results open up the possibility of targeting RBP4 as a new marker and potential therapeutic target for NAFLD,” closes dr xu
Let’s hope that the scientific community will resolve the existing conflicts by developing well-controlled experiments and large-scale clinical trials. Meanwhile, kudos to the researchers who identified the existing discrepancies and steered the research focus in the right direction.
Source:
Magazine reference:
Huang, H & Xu, C., (2022) Retinol-binding protein-4 and nonalcoholic fatty liver disease. Chinese Medical Journal. doi.org/10.1097/CM9.0000000000002135.
#Review #highlights #role #retinolbinding #protein4 #nonalcoholic #fatty #liver #disease

Leave a Comment