Tyler Griffin, The Canadian Press
TORONTO — Ontario’s top doctor says the province’s current monkeypox vaccination strategy is working and cases of the virus appear to be leveling off, but some working with people in shelters say the vaccination program should be expanded to better serve these communities .
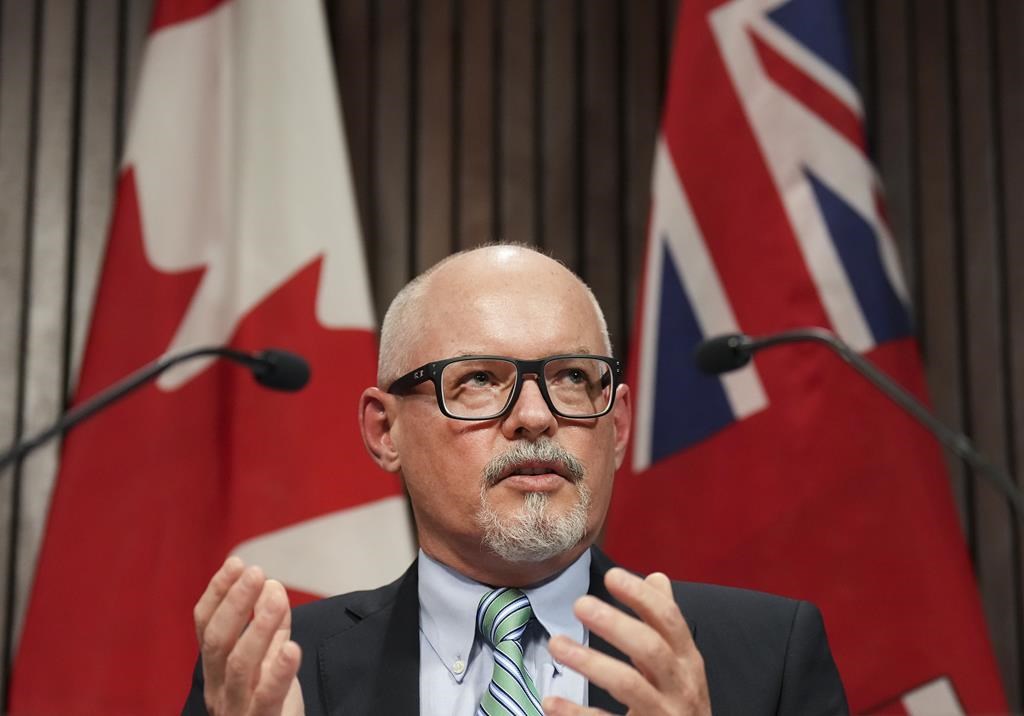
The Chief Medical Officer of Health, Dr. Kieran Moore said the province has so far vaccinated more than 20,000 people against monkeypox, with the priority group being gay, bisexual and other men who have sex with men who meet certain criteria.
“We’ve been able to source the vaccines we need from our federal partners, we’ve been able to staff our immunization clinics to meet the needs of our populations, we have the resources and the partnerships needed to ensure our health care system protects those affected by this virus.” are at risk,” Moore said in a recent interview.
“Our response in Ontario has been fairly robust. We still have a long way to go, but it seems that our overall number of (monkeypox) cases is stagnating on a plateau.”
But for some, the province’s vaccination strategy isn’t enough to protect those living in high-risk environments like homeless shelters, like a recently confirmed case of monkeypox in a person who visited a Toronto animal shelter.
Diana Chan McNally, a community worker at a center for people in need in Toronto, said she believes monkeypox vaccines should be widely available to people living in shelters as facilities come together and people living there may share property .
“This kind of laissez-faire attitude toward the vaccine is an integral part of the fact that we don’t seem to prioritize creating special protocols or really consider the unique conditions that can lead to monkeypox infection in the shelter system,” he said McNally.
She also said the current monkeypox vaccination strategy does not allow for overlap between people living in shelters and those who may be eligible for vaccination, such as sex workers and people in the LGBTQ community who are homeless and may not be Having access to the city, considered – operation of vaccination clinics.
“I don’t know why we can’t get dedicated amounts of the vaccine, even in small quantities, to the priority groups within the protection system,” she said. “I think that’s something that could potentially help reduce the risk of spreading.”
Chan McNally also said she would like to see the shot offered to the shelter workers. “If we protect their health, we can protect other people in the protection system,” she said.
Toronto Public Health held pop-up monkeypox vaccination clinics at the shelter where a case was recently reported, which Moore said is part of Ontario’s “ring immunization” strategy targeting those who may have been exposed to a known case.
Patricia Mueller, CEO of Homes First, the company that oversees the shelter where the case was confirmed, said there have been no other cases of monkeypox linked to this case. She said her staff, the city and Toronto’s public health department acted quickly to move the infected person to an isolation and recovery facility and set up a vaccination clinic.
Mueller added that shelter workers are considered to be at low risk for monkeypox infection.
Rita Shahin, associate medical officer of health at Toronto Public Health, said the city is not currently planning a major monkeypox vaccination program for all residents of the shelter, although those who meet the criteria are eligible for vaccination.
“We need to monitor where the disease is, who is most at risk, and if we see more cases or spread through the shelter system, we would certainly look at that,” Shahin said.
Shahin also said the city’s supply of monkeypox vaccines is “fairly limited,” though Moore said the province has a “significant reserve” of doses ready for emergency situations.
Thomas Tenkate, a professor in the School of Occupational and Public Health at Toronto Metropolitan University, said he agrees that men who have sex with men should remain the primary target for monkeypox vaccination because of transmission trends, but added, setting up pop-up clinics in emergency shelters could be a way to proactively contain the spread of the virus.
“If you’re going to vaccinate people in shelters, the strategies have to be different than those of the general public,” Tenkate said. “People who are using shelters or who are homeless, that’s where you really need to go.”
He said another challenge in vaccinating people in shelters is understanding their health history to identify potential complications from vaccination. “That could also be a limiting factor for implementation,” he said.
Public Health Ontario on Thursday reported a total of 449 confirmed cases of monkeypox in the province, up from 423 on Tuesday. The agency’s latest report says the majority of cases — more than 77 percent — were reported in Toronto.
It also says almost all of those infected are male, with only two reported in female patients. The virus generally does not spread easily and is transmitted through prolonged close contact via respiratory droplets, direct contact with skin lesions or body fluids, or through contaminated clothing or bedding.
— With files by Allison Jones.
This report from The Canadian Press was first published on August 8, 2022.
#Ontario #confident #monkeypox #vaccine #strategy #Moore #expand

Leave a Comment